Evaluation and Management Codes (commonly known as E/M Codes or E&M Codes) are Medical Billing Codes, used in processing health insurance claims by the health care providers in the USA, in order to get reimbursements by Medicare, Medicaid or private insurance for patient encounters.
Evaluation and Management standards and guidelines were established by Congress in 1995, revised in 1997. E&M Codes have been adopted by medical insurance companies as the standard guidelines for determining type and severity of patient conditions.
Evaluation and Management Codes are based on the Current Procedural Terminology (CPT) codes established by the American Medical Association (AMA).
In Medical Billing Evaluation and Management Codes, CPT codes, HCPCS codes and ICD-9-CM codes are used by medical coders to report patient treatment. The ICD-9-CM codes are also set to be replaced by ICD 10 Codes soon. The table below presents the commonly used codes during the various phases of treatment:
In 2010, new codes were added to the E&M Code set, for prolonged services without direct face-to-face contact. The new year brings changes to many evaluation and management codes physicians use, including chronic care management and advanced planning
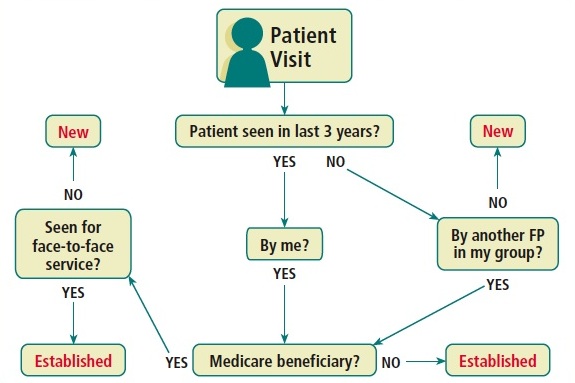
You can also learn correct use of CPT Code 99214 instead 99213 or 99212 for Evaluation and Management (E/M) Coding of Established Office Patient to increase revenue through legitimate Medicare reimbursement.
Evaluation and Management standards and guidelines were established by Congress in 1995, revised in 1997. E&M Codes have been adopted by medical insurance companies as the standard guidelines for determining type and severity of patient conditions.
Evaluation and Management Codes are based on the Current Procedural Terminology (CPT) codes established by the American Medical Association (AMA).
In Medical Billing Evaluation and Management Codes, CPT codes, HCPCS codes and ICD-9-CM codes are used by medical coders to report patient treatment. The ICD-9-CM codes are also set to be replaced by ICD 10 Codes soon. The table below presents the commonly used codes during the various phases of treatment:
- Assessment/ Brief Intervention
- Diagnosis
- Induction Day 1 and additional days
- Follow-up, Stabilization, and Maintenance
- Other coding options
In 2010, new codes were added to the E&M Code set, for prolonged services without direct face-to-face contact. The new year brings changes to many evaluation and management codes physicians use, including chronic care management and advanced planning
Evaluation and Management Codes Changes 2015
Three new codes have been added to the Evaluation and Management (E&M) section in 2015. These are in the Care Management and Advance Care planning subsections.Care Management Section
Care Management Services is new this year with extensive notes. This subcategory is for the management and support services provided by clinical staff, under the direction of a physician, to patients at home, in a domiciliary, or in assisted living.Chronic Care Management Services
"Complex Chronic Care Coordination" title has been changed to "Care Management Services" with an addition of a new subsection, “Chronic Care Management Services” to better reflect the management services described by new code 99490. This E&M code will be utilized to capture chronic care management services for the establishment, implementation, revision, or monitoring of the care plan for patients with at least two chronic conditions, expected to last at least 12 months, and may place the patient at risk of death, exacerbation, or functional decline. This code is reported if, during the calendar month, at least 20 minutes of clinical staff time is spent on care management activities.Advance Care Planning E&M Section
The two new advanced care planning codes (99497 and 99498) are used to report the face-to-face service between a physician or other qualified healthcare professional (QHCP) and a patient, family member, or surrogate in counseling and discussing advance directives, with or without completing relevant legal forms. The CPT manual defines advanced directive as:A document appointing an agent and/or recording the wishes of a patient pertaining to his/her medical treatment at a future time should he/she lack decisional capacity at that time.Advance Care Planning is a new subsection in the E/M section. Two E&M codes were placed in this subsection. The codes are used to report face-to-face discussion of advance directives:
- E&N Code 99497: Advanced care planning for the first 30 minutes
- E&N Code 99498: Add-on code assigned for each additional 30 minutes
- New and established patient office visits (99201-99215)
- Observation initial, subsequent and discharge care codes (99217-99220, 99224-99226)
- Initial, subsequent and discharge hospital service codes (99221-99233, 99238-99239)
- Observation or inpatient admit and discharge on the same date (99234-99236)
- Outpatient and inpatient consultations (99241-99255)
- Emergency department visit codes (99281-99285)
- Initial, subsequent and discharge nursing facility care codes (99304-99316)
- Annual nursing facility assessment code (99318)
- New, established and discharge domiciliary or rest home visit codes (99234-99337)
- New and established patient home visit codes (99341-99350)
- initial and periodic preventive medicine codes (99381-99397)
- Transitional Care Management Service codes (99495-99496)
- Critical care codes (99291, 99292)
- Inpatient neonatal and pediatric critical care codes (99468-99476)
- Initial and continuing intensive care services (99477-99480)
Prenatal Visit Guidelines
The maternity care and delivery guidelines were revised to specify the following:- Pregnancy confirmation during a problem-oriented or preventive visit is not considered a part of antepartum care. Report using the appropriate E/M code for that visit.
- Antepartum care includes the initial prenatal history and physical examination.
Social History Guidelines
E&M Guidelines for Social History has been expanded and will now include a bullet for Military History.You can also learn correct use of CPT Code 99214 instead 99213 or 99212 for Evaluation and Management (E/M) Coding of Established Office Patient to increase revenue through legitimate Medicare reimbursement.

Post a Comment
Webmaster reserves the rights to edit/remove comments that is found irrelevant, offensive, contain profanity, serves as spam or attempts to harbor irrelevant links. Please read our Comments Policy for details.