Medicare does cover Colon Cancer also referred as Colorectal Cancer, Rectal Cancer or Bowel cancer. Which is the development of cancer in the colon or rectum in the lower part of the large intestine. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body.
Colon Cancer Symptoms and Signs include blood in the stool, a change in bowel movements, weight loss, and feeling tired all the time.
In US, Colon Cancer Screening is found effective to decrease colon cancer related deaths. Colon Cancer Screening is recommended starting at the age of 50 and continuing until the age of 75 in United States.
However, there is an exception to this. For colonoscopy procedure (which can also diagnose colon cancer) there is no minimum age requirement.
Below are the medicare colon cancer screening coverage eligibility guidelines:
From 2012, Medicare Advantage Plans will cover all preventive services the same as Original Medicare. This means Medicare Advantage (MA) plans will not be allowed to charge cost-sharing fees (coinsurances, copays or deductibles) for preventive services that Original Medicare does not charge for as long as you see in-network providers. If you see providers that are not in your plan’s network, charges will typically apply. Therefore, if you are in a Medicare Advantage plan, contact your plan to find out what rules and costs apply.
For Barium Enema, patient will pay 80 percent of the Medicare approved amount if the doctor takes assignment. The Medicare Part-B deductible does not apply.
For Diagnostic Colon Cancer Screening, if a patient undergoes colonoscopy and the provider finds and removes a polyp, the costs will apply. Patient would have to pay the coinsurance for the colonoscopy and the polyp removal because the Colon Cancer Screening became diagnostic. However, no deductible will apply.
Colon Cancer Symptoms and Signs include blood in the stool, a change in bowel movements, weight loss, and feeling tired all the time.
Colon Cancer Screening
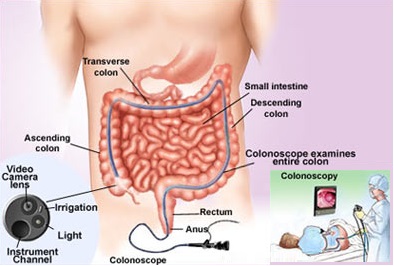
Colon Cancer Screening can be done by obtaining a sample of the colon during a sigmoidoscopy or colonoscopy. This is then followed by medical imaging to determine disease spread, colon cancer staging and prognosis.In US, Colon Cancer Screening is found effective to decrease colon cancer related deaths. Colon Cancer Screening is recommended starting at the age of 50 and continuing until the age of 75 in United States.
Colon Cancer Screening Medicare Coverage Guidelines and Codes
You can checkout the Colorectal Cancer Screening ICD 9 and CPT Codes under which Medicare does cover colorectal (colon) cancer screenings.Medicare Colon Cancer Screening Coverage Guidelines
With Medicare, a patient must be 50 age or older to be eligible for Medicare Colon Cancer Screening Coverage for most of the colon cancer types.However, there is an exception to this. For colonoscopy procedure (which can also diagnose colon cancer) there is no minimum age requirement.
Below are the medicare colon cancer screening coverage eligibility guidelines:
- Fecal occult blood test - once a year (every 12 months) for persons age 50 or older.
- Flexible sigmoidoscopy - once every four years (48 months) for persons at high risk and less frequently for other persons.
- Colonoscopy - once every two years (24 months) if you are at high risk for colorectal cancer (Have a family history of the disease or have had colorectal polyps or colorectal cancer, or have had inflammatory bowel disease).
- Medicare covers colonoscopies every 10 years (but not within 48 months of a screening flexible sigmoidoscopy) if you are not at high-risk.
- Barium enema – once every two years for persons at high risk and once every four year for others (but not within 48 months of a screening flexible sigmoidoscopy).
From 2012, Medicare Advantage Plans will cover all preventive services the same as Original Medicare. This means Medicare Advantage (MA) plans will not be allowed to charge cost-sharing fees (coinsurances, copays or deductibles) for preventive services that Original Medicare does not charge for as long as you see in-network providers. If you see providers that are not in your plan’s network, charges will typically apply. Therefore, if you are in a Medicare Advantage plan, contact your plan to find out what rules and costs apply.
For Barium Enema, patient will pay 80 percent of the Medicare approved amount if the doctor takes assignment. The Medicare Part-B deductible does not apply.
For Diagnostic Colon Cancer Screening, if a patient undergoes colonoscopy and the provider finds and removes a polyp, the costs will apply. Patient would have to pay the coinsurance for the colonoscopy and the polyp removal because the Colon Cancer Screening became diagnostic. However, no deductible will apply.

Post a Comment
Webmaster reserves the rights to edit/remove comments that is found irrelevant, offensive, contain profanity, serves as spam or attempts to harbor irrelevant links. Please read our Comments Policy for details.